As a hospital social worker for several years, my role was to help patients and families plan for discharge and coordinate care. Discharge planning is the process of assessing patient needs and goals, planning treatment, and coordinating care.
Understanding your discharge options for care can help you collaborate with your treatment team to make sure you have the best care after you discharge from the hospital. The goal of discharge planning is to ensure you have a smooth transition to a successful recovery.
In this post I’ll be covering the following:
- Why Discharge Planning is Important
- What You Can Expect When Working with a Discharge Planner
- Your Post Hospital Discharge Options
Why Discharge Planning is Important
It may surprise you, but discharge planning happens on the day of admission.
It’s important to plan for discharge as soon as possible because care coordination takes a lot of time as there are a lot of moving parts.
On average a hospital stay is about 3-4 days. A hospital provides short-term acute care for patients with the intent of getting them stable enough to receive further recovery and treatment.
Coordinating care for a patient’s discharge includes:
- talking to the patient
- talking to families
- talking to the treatment team
- working with health insurance companies
- and working with community agencies and facilities
It can be time consuming and hectic, which is why it’s important to start the planning process on the day of admission to the hospital.
When a social worker or case manager meets with you for the first time, they are wanting to discuss potential discharge options with you so that your transition to care is as smooth as possible.
We don’t want to be running around like chickens with our heads cut off, trying to make miracles happen. (Myth Buster: Social Workers are NOT miracle makers)
Communicating with your treatment team and discharge planner on a regular basis is vital to make sure your goals are met and you receive the most appropriate post hospital discharge option for your care.
What You Can Expect When Working with a Discharge Planner

Your discharge planner may be a social worker or a nurse case manager. They usually try to see you within the first 24-48 hours of your hospital admission. You can expect that your discharge planner will want to start talking to you about potential discharge plan options.
This is not because they want to kick you out of the hospital.
I promise.
It’s because they want to start the planning process so that there are less complications and bumps to your recovery.
When I meet with patients, I understand that we may not know what the treatment plan is within the first 24-48 hours of admission. So, I talk with patients about the “possible” or “potential” discharge options and plan for all possibilities.
Hopefully all hospital discharge planners take this approach.
They should be talking to you about all possible options for discharge care.
Planning for possible Acute Rehab, Skilled Nursing Facility, Home health care, etc., all at the same time can help set your discharge up for success, even if the treatment team isn’t sure which plan to recommend yet.
This way when it finally is time for discharge, your care is already set up and you don’t have to continue to wait around in the hospital.
Your Post Hospital Discharge Options
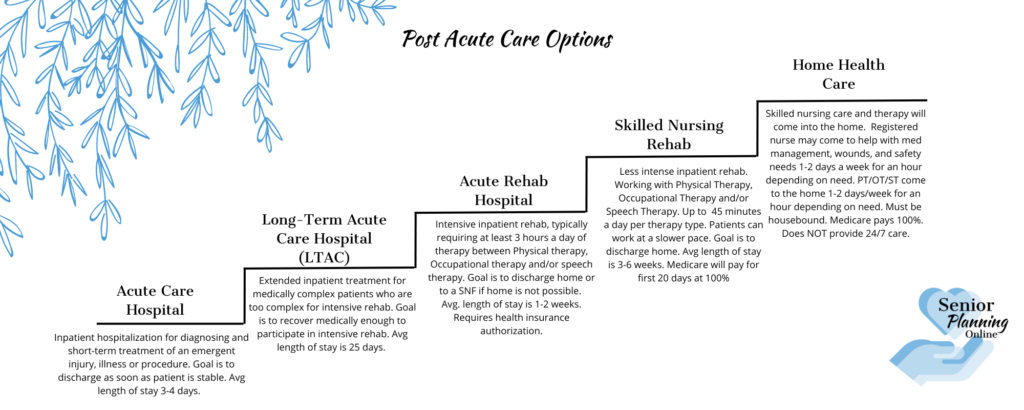
There are different levels of care that you can discharge to. The care option you discharge to all depends on the patient’s and family’s goals, the recommendations made by the treatment team and the patient’s health insurance plan.
Each discharge options offers a different level of care. I’ll briefly describe what each discharge option is. You can click the options below for a more in-depth overview of each type.
Long-Term Acute Care Hospital
Acute Rehab Hospital
Skilled Nursing Rehab
Home Health Care
Hospice and Palliative
Long-Term Acute Care Hospital (LTAC)
A Long-Term Acute Care Hospital is often known by its acronym LTACH or LTAC.
An LTAC provides intensive care for patients who are medically complex and need a longer time to recover in a hospital setting.
The focus of an LTAC is more medical, though they can provide some rehab services. However, an LTAC’s goal is to get the patient to a stable enough condition where they can participate in more intensive rehab care. The average length of stay for an LTAC is 25 days.
Acute Rehab Hospital (ARF/AR)
An acute rehab hospital provides intensive rehabilitation care. They can provide some complex medical care, but the patient needs to be able to participate in a minimum of 3 hours of rehab therapy per day. The focus is rehabilitation to get back to independent functioning and living. The average length of stay is about 1-2 weeks.
Skilled Nursing Rehab (SNF)
A skilled nursing facility or SNF, provides both medical care and rehabilitation care for patients who are not too medically complex. Patients have skilled nursing needs AND have the ability to participate in daily rehabilitation. The rehabilitation patients receive at a SNF is not as intensive as an Acute Rehab Hospital. However, this allows for a patient to recover at a pace they can tolerate. The average length of stay is 2-6 weeks.
Home Health Care
Home Health Care provides skilled care and rehabilitation in the home setting. It provides skilled nursing care for less complex medical needs and some rehabilitation that is not as intensive as a Skilled Nursing Facility (SNF). These services are provided 3-5 days a week for about an hour per discipline.
Individuals must be safe enough to go home, but may still have some limited medical and rehab needs. Home Health care can be provided at home for as long as progress is being made and for as long as insurance will approve it.
Senior Living Placement
Sometimes patients admit to the hospital and it is determined that they are not safe to go back to their previous living environment. They may not qualify for intensive rehabilitation care, or maybe they simply just need more care than what family can provide. In these situations, social workers and case managers may be able to help find senior living or long-term placement, with the help of the family. Finding Senior Living Placement should really start and take place by the family and before a hospitalization happens.
However, there may be exceptions where it’s not safe for the patient to remain home with the family member and there are no other options. Especially with regards to dementia diagnoses. Behaviors can be difficult and so family may need some extra assistance.
Hospice & Palliative Care
Palliative care may be recommended by the doctor for patients who come in with a chronic illness that may need some extra outpatient support and pain management. Palliative care is a good option for those who have a chronic illness but still want to seek treatment options and need symptom management.
Hospice care at home or a Hospice home/Hospice inpatient care may be recommended for patients who have a terminal illness. Patients with a terminal illness may no longer want to seek treatment options and instead their focus is more for comfort care. Hospice either in the home or going to a specific facility that has inpatient hospice may be the best discharge plan.
Conclusion
As you can see there are several discharge options that may be discussed or recommended by your acute care hospital team. Having regular communication with your treatment team and asking questions is important so that you can be involved in deciding which discharge option is best for you or your loved one.


No responses yet