Hospice care and palliative care are often used interchangeably. However, their approaches to care are quite different. Hopefully you gained a better understanding about what palliative care is by reading our post “The Truth About Palliative Care“.
So let’s dive into what hospice care actually is, what the benefits are and how to qualify for hospice.
What is Hospice?
Hospice is a specialized healthcare team focused on providing comfort and symptom management for someone who is terminally ill. According to CMS regulations, terminally ill means the individual has a medical prognosis of a life expectancy of 6 months or less.
This means the person has reached the end-stages of the disease process and no longer has curative treatment options.
At this point, the goal is to help the person be as comfortable as possible as they live out their final days of the disease process. This could be days, weeks or even months.
Hospice agencies have a team of healthcare professionals that specialize in the end-stages of life. A Hospice physician or nurse practitioner often takes over the patient’s care. They work with nurses, social workers and spiritual care providers to meet all of the patient’s needs as they near the end of life.

How to Qualify for Hospice Care
So when is Hospice care recommended and how do you qualify?
A patient may qualify for Hospice care if they are given a terminal diagnosis with a life expectancy of 6 months or less based on the progression of the diagnosis.
In addition to their 6 months to live prognosis, a patient will also need to show that they need physical help with about 3 activities of daily living.
Activities of daily living (ADLs) can include:
- Bathing/showering
- Getting dressed
- Personal hygiene (face-washing, brushing teeth, and caring for hair)
- Toileting needs (getting to and from the bathroom, getting on and off the toilet, wiping or changing of attends/depends)
- Ability to feed oneself
- Being able to sit, stand or walk
Some other qualifications can include a cognitive decline showing the patient does not have the capacity to understand their diagnosis, unable to handle day to day tasks like finances etc.
Additionally if the patient has had over 3 hospital visits in the last 4-6 months or a 10% or more body weight loss over the last 4-6 months.
It’s important to note that not everyone will meet every single one of these qualifications in order to be considered hospice eligible. These are guidelines.
Make sure you ask your medical care team for a hospice consult if you feel that you or your loved one might meet ANY of these criteria.

What Does Hospice Do?
As mentioned previously, hospice is focused on providing comfort care, not a cure for the disease or illness.
Similarly to palliative care, they offer a team of healthcare professionals that include a physician, nurse, social worker, home health aide and spiritual support. This team will be managing symptom, promoting comfort and quality of life, offering emotional and spiritual support and helping families cope after their loved one has died.
Symptom Management
Hospice providers offer relief of pain or other uncomfortable symptoms of the disease often through medication management.
They will evaluate the patient’s pain and other symptoms. Then they will prescribe medication to alleviate these symptoms as often and as frequently as needed to relieve pain and stress for the patient.
Certain medical equipment is also provided to help keep the patient as comfortable as possible, Medical equipment can include:
Oxygen, a hospital bed, wheelchair, walker, bedside commode, continence care supplies, and wound care needs.
Comfort vs Curing
Hospice can provide any equipment or medication needed to keep the patient comfortable. Hospice does NOT provide medications or equipment that is used for curative measures.
Remember, the goal is NOT to cure the patient, but instead to provide relief as they live out their last days.
Sometimes patients are put on medications to help with an infection. One question I often get is related to the use of antibiotics. People ask me if a patient has an infection and needs antibiotics, will Hospice cover this?
If the antibiotics will help alleviate any discomfort, then yes, it can be covered under hospice. If the antibiotics are only going to extend a patient’s life and the patient is not in discomfort or pain with the use of antibiotics, then it is NOT covered by hospice.
This can also be applied to any medication a patient is on.
The hospice provider will likely go through a patient’s medication regimen and discontinue any medications that are unnecessary and do not help with symptom management.
Promoting Quality of Life
Hospice agencies are often available on-call 24/7. This DOES not mean the care providers physically stay with the patient 24/7.
Instead, they are on-call. If a patient is in a lot of pain or having any other symptom concerns causing discomfort, the patient or family member can call the hospice agency. The hospice agency will either walk the patient or family member through the care needed or they will send a nurse out to help.
Promoting quality of life also means helping the patient have as much dignity as possible during the dying process. This often means providing a home health aide to assist the patient with some of their personal care needs.
The home health aide can help with bathing, personal hygiene and sometimes dressing. Most of the time a home health aide can only come out a few times a week. But discuss this option with the hospice provider to find out how often they can offer this assistance.
Emotional and Spiritual Support
One of the most difficult aspects of end of life care is the emotional and spiritual suffering the patient and family are experiencing.
There are so many emotions that both the patient and family are experiencing. Anything from fear of death or fear of the unknown, anger with the reality of the illness, guilt and regret, depression and anxiety, and every feeling in between are experienced.
Hospice offers a social worker to help patients and families work through these feelings, find strategies to cope and to give overall emotional support.
As people near the end of life, their religious and spiritual sense of self are affected. Hospice can offer a chaplain to help patients and families navigate their feelings and help them find meaning in life or in death. You don’t have to be connected to a religion to receive spiritual support from a chaplain.
Chaplains are trained and knowledgeable in almost every religion or spiritual belief. They are there to help people find comfort, solace, peace, hope and acceptance.
If you are religious and have certain religious preferences or rituals, Chaplains can help you incorporate these into your last days and afterwards. They can also help the patient and family with funeral and burial preparations.
Bereavement Care and Counseling
One of the most unique things about Hospice care, is the services that are available to families after their loved one dies.
Hospice care extends to family even after the patient has died. Bereavement services and counseling is offered to the family. Some agencies offer grief counseling for several months after the patient has died.
The loss of someone is devastating, even if it was expected. Bereavement and counseling care can help families cope with the many stages of grief. It can be given on an individual basis with each family member or to the family as a whole.
Hospice Care Options
Hospice services can be offered in a few different settings. Let’s go over what these options are:
Hospice at Home
Some patients and families prefer to have hospice services provided at home. They are able to live out their moments in the comfort of their own home. If this is an option you or your loved one are looking into, here are a few things to know.
The hospice agency of your choice will help you get set up in your home. There is a coordinator and an admissions nurse that will work on getting the equipment needed.
Equipment such as a hospital bed, bedside commode, wheelchair, walker, home oxygen and patient lifts are all provided by hospice. The patient will be evaluated by the coordinator and nurse to help determine what equipment will be needed in the home.
For more information on the different types of Medical supplies and equipment that are available, check out the post “A List of Medical Supplies and How You Can Get Them“.
The nurse and hospice coordinator will order the necessary equipment and arrange delivery and set up of the equipment. They will also educate the patient and their family on how to operate all of the equipment.
In addition to equipment, hospice also provides incontinence supplies like attends and depends. This is helpful for the family so that they don’t have to spend more money on these supplies.
Often families and patients assume that hospice in the home means they will get 24/7 care in the home. This is not the case.
The hospice agency is able to provide a nurse that can come out for an hour or 2 daily if needed. The patient and family has 24/7 access to a hospice nurse by phone, however, the nurse is not able to be in the home 24/7.
A hospice nurse may be scheduled to make visits every other day, daily visits and sometimes more frequent visits depending on the symptomatic needs of the patient. As the patient nears the end of their life and they become more imminent, the hospice nurse is usually able to be there with the patient and family the entire time. This could be several hours or more.
In addition to a nurse, a nursing aide or caregiver is available to come and bathe the patient at home 2-3 days per week. They can also help with personal hygiene needs, changing and dressing while they are there. These nursing aides /caregivers are typically only available for an hour or 2 a few times a week depending on the needs of the patient.
Patients and families also have access to hospice social workers and chaplains. They are able to visit for an hour or so as frequently as needed. The social worker and the chaplain’s role are available for emotional and spiritual support and to help with resources and ancillary needs.
Hospice in a Nursing Home or Assisted Living Facility
If the patient resides in a nursing home or assisted living facility, they absolutely can still receive hospice services!
In fact, I tell patients and families that having hospice in a facility is adding an extra layer of support for the patient.
The patient will still receive the same care they were receiving in the nursing home or assisted living facility. That should never change. If the patient was receiving total assistance with care by the nursing staff at the facility, that will continue.
Instead, hospice adds more help. They can still have a nurse’s aid come and give additional bathes or help with personal hygiene needs a few times a week. The nursing home should still be bathing the patient as usual, but hospice can give extra days of bathing if it’s something the patient wants. They can also spend a little bit of time with the patient for companionship a few times a week.
The hospice nurse will still be making frequent visits to the patient in the facility. The nurse is there to ensure the patient is comfortable and getting the care they need. They make sure their pain and other symptoms are controlled and can work with the patient’s hospice physician and nursing home physician to make any accommodations.
Similar to hospice at home, a social worker and chaplain is available to the patient within their nursing home or assisted living facility.
Inpatient Hospice or Hospice House

Another option of receiving hospice care is utilizing inpatient hospice or a hospice house.
A hospice house or inpatient hospice unit in a hospital are places of care dedicated to hospice care. A hospice house can be a stand-alone facility or a unit inside another medical building like a hospital.
These hospice houses try to emmulate a home-like and peaceful environment for the patient to die in. It has 24/7 nursing and medical care similar to a nursing home. The biggest difference is that the staff are dedicated to comfort and there are usually more nursing staff available for the patient than at a typical nursing home.
The nursing staff at hospice houses are specifically trained for hospice care and comfort. They understand the dying process on more than a medical standpoint, but they also understand the emotional and spiritual struggles.
There are also chaplains and social workers available in the hospice house as well. Providing the additional layer of support to the patient and their family members.
Often, a hospice house also has an area for family to convene or sometimes a small space in the patient’s room for a family member to stay the night.
In my experience, the hospice houses I have personally been to are very peaceful, clean and inviting.
What you need to know about this option is that this is really only available for someone who is at the very end stages of their disease process and they are in the imminent stage. This means that they likely have less than 2 weeks to live and who are symptomatic.
This means that the patient may be having severe pain that is difficult to control in a home or nursing home environment and demands intravenous (IV) medication management. They also might be experiencing extreme anxiety, difficulty breathing that cannot be managed at home.
Who Pays for Hospice Care?
All of the above hospice services we just went over can be covered by insurance. It just depends on your insurance plan.
If you have traditional/original Medicare part A and B (or even just Medicare part A), hospice is completely covered 100%. There are no out of pocket expenses or co-pays to worry about.
If you have a Medicare advantage or replacement plan, these plans usually have a hospice benefit as well. Because these plans are managed plans, they are still part of Medicare. This means they are required by Medicare to provide the hospice benefit.
If you want to know the difference between Traditional Medicare and the Medicare Replacement plans, check out our post “What No One Tells You About Medicare Enrollment“.
So if you have Humana Medicare, United Healthcare Medicare, Kaiser Medicare, Aetna Medicare, Blue cross blue shields Medicare, etc…all of hospice care should be covered 100%.
If you have a commercial insurance plan, usually through an employer or purchased through the market place, you may need to contact your insurance plan to ensure they have a hospice benefit. Sometimes they will have the hospice benefit, but there may be a copay associated with it.
Insurance like Tricare and VA benefits also provide the hospice care benefit without copays or out of pocket expenses.
If you have Medicaid through your state, hospice care is also built into your Medicaid insurance. Hospice care should be covered at 100% under Medicaid. You can check in with the Medicaid insurance plan to be sure.
What if you don’t have Insurance?
You can still receive hospice care even if you don’t have any insurance plan. Many hospice agencies try to work with families on either a payment plan, help apply for Medicaid or will look into a charity or foundation to help pay for the care.
Check with the hospice agency you are working with to find out what your options are if you don’t have any insurance coverage.
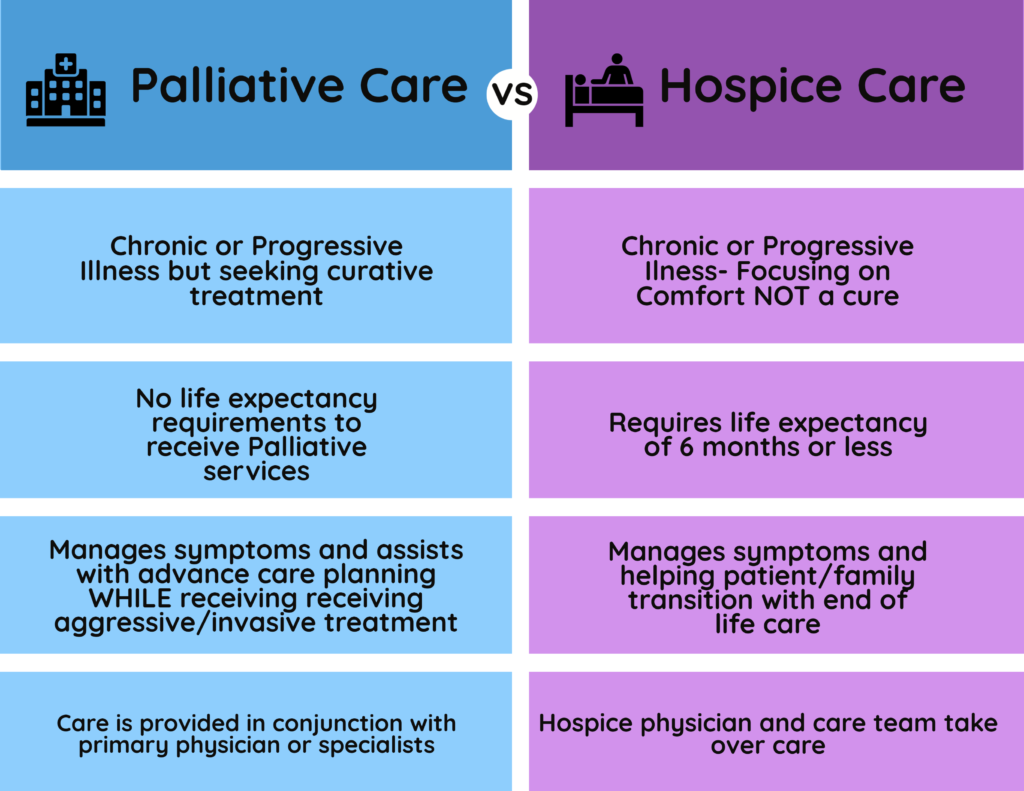
The Difference Between Hospice Care vs Palliative Care
Hopefully you read our post on “The Truth About Palliative Care“ and have a better grasp on what it is.
Although palliative care and hospice care are often talked about as the same service, they are quite different.
Palliative care can be used as precursor to hospice care. Typically people who have a chronic or progressive diagnosis are still seeking treatment options. They may not be at the end-stages of their disease process. However, as the disease progresses and their treatment options decline, it might be time to consider Hospice care.
Hospice care continues the comfort, symptom management and emotional support that had been given while the person was still seeking curative treatments. However, now the focus for comfort is more intense and more of a priority.
The Bottom Line
To sum everything up, Hospice care is a healthcare service that provides comfort and symptom management for people who typically have a prognosis of 6 months or less of a terminal illness. Their goal is to ensure comfort for the patient as they live out their last days. At this point, the patient is no longer looking to receive curative treatment.
A hospice care team typically consists of an overseeing Hospice physician, nursing staff, social workers and chaplains to address the patient’s needs as a whole.
Hospice care can be provided in the home, at a nursing home or assisted living facility or in a dedicated hospice house.
Most insurances pay for hospice care services but it’s important that you contact your specific insurance plan to make sure there aren’t any copays or deductibles that would need to be met.
Hospice care is not just helpful for the patient who is in the end stages of their disease process, but it can be a great tool and benefit for families. The hospice care team isn’t just there for the patient, but also for the family, offering emotional and spiritual support throughout the disease process and even after the patient has died.
To find a hospice care agency in your area, check out the Hospice Search feature on Medicare.gov’s website!


One response
Thanks for helping me understand that hospice care is specifically made to help people that received a terminal disease diagnosis. I was curious why one of the characters on a show I was watching called out a hospice care expert after being diagnosed with stage 4 cancer. I’ll probably consider this too if ever it happens to my loved ones or me.